Understanding Epilepsy
- What you need to know about epilepsy?
- Epilepsy and pregnancy
- Myths and facts
- What to do if someone has a seizure
- Working with epilepsy
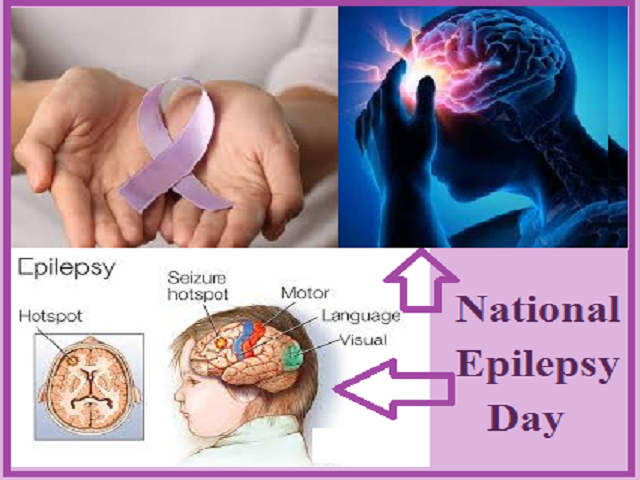
Human brain is made up of billions of nerve cells or neurons. These neurons communicate through electrical and chemical signals. When there is any fault in the nerve cells, there is a sudden excessive electrical discharge that disturbs the normal activity in the brain. Abrupt and increased electrical discharge in the brain results in epilepsy, also known as a seizure disorder.
WHAT HAPPENS DURING A SEIZURE ATTACK?
During seizures, the person may become unconscious, fall on the floor and jerk violently for several minutes. This might last for few minutes and later the nerve cells start to behave normally, and the person returns to normalcy.
Epilepsy doesn’t discriminate anyone. Epilepsy affects both males and females of all races, ethnic backgrounds and ages. People of all ages may suffer from epilepsy. The condition can begin at any age, although its onset is most often in childhood or in the later years of life.
BURDEN OF EPILEPSY
Epilepsy is the second most common and frequently encountered neurological condition. It imposes heavy burden on individuals, families and also on healthcare Systems. In India, >10 million people suffer from epilepsy. Nearly 70 Million people around the world suffer from epilepsy.80% of the people with epilepsy live in low- and middle-income countries. In India, the prevalence of epilepsy is higher in the rural compared to urban population.
What causes epilepsy?
Some types of epilepsy are inherited genetically i.e. they run-in families. Infectious diseases, such as meningitis, AIDS and viral encephalitis. Brain damage that occurs before birth due to infection in the mother; poor nutrition or oxygen deficiencies. Stroke is a leading cause of epilepsy in elderly population. In 50% of the Cases, the cause of epilepsy is not identifiable or unknown. In the other 50%, the Condition may be due to various factors.
FACTORS THAT TRIGGER EPILEPSY
The likelihood of having a seizure at some point may include the following reasons
Medication-related
- Missing medication
- Additional medications taken with anti-epileptic medication
Internal factors
- Stress, excitement and emotional status
- Lack of sleep
- Fever
- Menstrual cycle
External factors
- Alcohol and smoking
- Poor diet
- Very warm weather, hot baths or showers
- Television, videos and flashing lights
Knowing what triggers your seizures can help you recognize when a seizure may occur and help you be prepared.
WHAT ARE THE SYMPTOMS OF EPILEPSY?
The main symptom of epilepsy is repeated seizures. Seizures can affect people in different ways, depending on which part of the brain is involved. Some seizures cause the body to jerk and shake, while others cause problems like loss of awareness or unusual sensations. The common symptoms of epilepsy include
- Confusion
- Aura-An’aura’ is the term some people use to describe the warning they feel before they have a seizure
- Sudden falls
- Staring
- Uncontrollable Jerking movements
- Strange Sensations and emotions
- Loss of consciousness or awareness
Most of the time, a person with epilepsy will tend to have the same type of seizure each time, so the symptoms will be similar from episode to episode.
WHEN TO SEEK MEDICAL ATTENTION?
If someone is having epileptic seizures, reach out to the nearest hospital or call an ambulance
- A seizure lasts for 5 minutes or longer.
- One seizure occurs right after another before the person regains the consciousness.
- Breathing becomes difficult or the person appears to be choking.
- The seizure occurs in water.
- Injury may have occurred.
- The person asks for medical help.
WHAT ARE THE TYPES OF SEIZURES?
There are different types of seizures. Generally, they are categorized based on what part of the brain is involved in a seizure. People might experience one type or more than one type of seizures.
1.Generalized seizures
- Entire brain is affected
- The person is unconscious
2.Focal seizures
- One area of brain is affected
- The person may have impaired consciousness or be fully active
3.OTHER TYPES
Non-epileptic seizures
Not related to epilepsy Caused due to diabetes, high fever or other medical conditions
Status epileptics
: Continuing seizure
Last >30 min, or two or more seizures without full recovery of consciousness between any of them
TYPES OF GENERALIZED SEIZURES
20% of people with non-epileptic epilepsy experience
60% of seizures (NES) epilepsy seizures are focal seizures
30% of people with epilepsy experience generalized seizures
ABSENCE SEIZURES
- Stare blankly into space and be unresponsive
- Usually for 5 to 10 seconds
MYOCLONIC SEIZURES
- Brief jerks of a muscle involving the neck, shoulders and upper arms
ATONIC SEIZURES
Sudden loss of muscle strength
The person may fall to the ground
Usually lasts less than 15 second
TONIC CLONIC SEIZURES
- Body briefly stiffens followed by a jerking motion of the arms and legs
- Loss of consciousness and falls occur frequently
- Excessive saliva production may be present
- Lasts a couple of minutes
TONIC SEIZURES
- muscles rapidly constrict
- limbs and body may become rigid
- person may fall to the ground usually backwards
- last for less than minute
DIAGNOSIS OF EPILEPSY
The presence of epilepsy depends on the symptoms before, during and after seizure. Doctors gather lots of different information to assess the causes of seizures If you have a seizure you may not remember what has happened. It can be helpful to have a description of what happened, from someone who saw your seizure, to pass on to your doctor or a specialist.
Here are some questions that may help you or someone who witnessed your seizure to record useful information about what happened.
BEFORE THE SEIZURE
- Did anything trigger (set off) the seizure – for example, did you feel tired, hungry, or unwell?
- Did you have any warning that the seizure was going to happen?
- Did your mood change – for example, were you excited, anxious or quiet?
- Did you make any sound, such as crying or mumbling?
- Did you notice any unusual sensations, such as an odd smell or taste, or a rising feeling in your stomach?
- Where were you and what were you doing before the seizure?
DURING THE SEIZURE
- Did you appear to be ‘blank’ or stare into space?
- Did you lose consciousness or become confused?
- Did you do anything unusual such as mumble, wander about or fiddle with your clothing?
- Did your colour change (become pale or flushed) and if so, where (face or lips)?
- Did your breathing change (for example, become noisy or seemed difficult to breathe)?
- Did any part of your body move, jerk or twitch?
- Did you fall down, or go stiff?
- Did you wet yourself?
- Did you bite your tongue or cheek?
AFTER THE SEIZURE
- How did you feel after the seizure did you feel tired, worn out or feel sleepy?
- How long was it before you were able to carry on as normal? Did you notice anything else?
HISTORY AND PHYSICAL EXAMINATION
Your doctor will start reviewing your medical and family history to see if seizures run in your family and asking about the symptoms you have experienced. You will probably also have a physical exam so that your doctor can check to see if there’s an underlying medical condition that is causing your seizures. Doctors ask people about possible causes of seizures, such as the following:
Whether people have had a disorder that can cause seizures (such as a brain infection) or a head injury
Which drugs (including alcohol) they are taking or have recently stopped
For people who are taking drugs to control seizures, whether they are taking the drugs as directed
Whether they are getting enough sleep (not getting enough sleep can make seizures more likely to occur in some people)
YOUR DOCTOR MAY ORDER A NUMBER OF TESTS TO HELP WITH A DIAGNOSIS
NEUROLOGICAL EXAM
A neurological exam me involve testing your reflexes balance muscle strength coordination And your ability to feel this can help the doctor to determine what type of epilepsy you have
BLOOD TESTS
Blood tests are done to check for signs of infections, genetic conditions or other conditions that may be associated with seizures. Also, to determine if kidneys, thyroid, and other organs are functioning properly and that they are not the cause of seizures.
ELECTROENCEPHALOGRAM
Electroencephalogram (EEG) is a painless, safe procedure that records electrical activity in the brain. Doctors examine the recording EEG to check for abnormal electrical discharges. In this test, electrodes are attached to your scalp with a paste-like substance or cap. The electrodes record the electrical activity of your brain.
COMPUTEDTOMOGRAPHY SCAN-This test helps identify blood clots, cysts, brain tumours, scar tissue or other problems that can cause seizures.
MAGNETIC RESONANCE IMAGING (MRI)-This test is used to identify structure and abnormalities within the brain.
EEG-VIDEO MONITORING
EEG-video monitoring is an even better diagnostic method. During this type of monitoring, an EEG monitors the brain’s activity and cameras videotape body movements and behaviour during a seizure.
Prolonged monitoring often requires the patient to spend time in a special facility for several days. Prolonged EEG-video monitoring is the only definitive way to diagnose epilepsy
Treatment of epilepsy.
After diagnostic confirmation of epilepsy, there are many ways to get treated. They usually include; medication or drug to control seizure, a special diet, an implant which can work on the brain or nerves and surgery that could help the patient feel better.
MEDICATION THERAPY-The majority of epileptic seizures are controlled through drug therapy. Treatment is usually with antiepileptic drugs (AEDs) or anti-convulsant drugs. The type of treatment
Prescribed will depend on several factors including the frequency and severity of the seizures as well as the person’s age, overall health and medical history. An accurate diagnosis of the type of epilepsy is also critical in choosing the best treatment. Although the different types of epilepsy vary greatly, in general, medications can control seizures in about 70% of epilepsy patients.
Anti-epileptic drugs are usually started at lower doses and increased gradually. In some cases, combination of drugs is prescribed. The action of the drug might vary from person to person.
POINTS TOREMEMBER WHILE ON MEDICATION
- Take medications exactly as prescribed.
- Regular medical reviews are recommended, and many people need medication for a limited time, usually a few years.
- Do not suddenly stop a taking medication, as this can provoke Seizures and possibly medical emergency
- Withdrawing from medication should always be carried out under the consulting physician or a medical supervision.
- Any changes to dose should be guided by the treating doctor.
- Notify your doctor immediately, if you notice new or increased feelings of depression, suicidal thoughts, or unusual changes in your mood or behaviours.
SIDE EFFECTS WITH ANTIEPILEPTIC MEDICATIONS
As it is true for all drugs, the drugs used to treat epilepsy have side effects. The occurrence of side effects depends on the dose, type of medication and length of treatment. The side effects worsen with doses but tend to be less severe with time as the body adjusts to the medication.
Mild side effects may include:
Fatigue ? Skin rashes, Dizziness, Weight gain, Loss of bone density,? ? Speech problems, . Memory and thinking problems, Loss of coordination
More severe but rare side effects may include:
Depression, Suicidal thoughts and behaviours, Severe rash? Inflammation of certain organs, such as liver
DIETARY THERAPY –Dietary therapy is an approach to help control seizures, usually in conjunction with seizure medications. The classic ketogenic diet, a special high-fat, low-carbohydrate diet, are prescribed
and monitored by a physician and nutritionist and can help control seizures in some people. It can help both children and adults with refractory seizures.one can initiate ketogenic diet by removing the regular diet and replacing with higher fat, adequate protein, lower carbohydrate diet. However, please contact your doctor and dietician before starting the diet. Seizure reduction can occur very soon after the ketogenic diet is initiated. In some cases, it may take several months. However, commitment to consistency of diet intake is important to determine the effectiveness of the therapy in controlling seizures. Side effects of a ketogenic diet may include dehydration, constipation, slowed growth because of nutritional deficiencies and a build-up of uric acid in the blood, which can cause kidney stones. These side effects are uncommon, if the diet is properly and medically supervised.
SURGICAL THERAPY
Epilepsy surgery is a procedure that removes or alters an area of your brain where seizures originate. Epilepsy surgery is most effective when seizures always originate in a single location in the brain.
Epilepsy surgery is not the first-line of treatment but it is considered when at least two anti-seizure medications have failed to control seizures. the goal of epilepsy surgery is to eliminate seizures or limit their severity with or without the use of medications
Types of epilepsy surgery
Resective surgery: It is the most common epilepsy surgery, that involves the removal of a small portion of the brain. The surgeon cuts out brain tissues in the area of the brain where seizures originate.
Laser interstitial thermal therapy (LITT): This is a less invasive surgery that uses a laser to pinpoint and destroy a small portion of brain tissue.
Deep brain stimulation: In this procedure, an electrode is permanently placed in the brain that releases electrical signals at regular interval and disrupts abnormal Inducing activity the generator sending the electrical pulse is implanted in the chest.
Corpus callosotomy: Corpus callosum is the bundle of nerves connecting the right and left sides of the brain. Corpus callosotomy is a surgical procedure that cuts the corpus callosum, interrupting the spread of seizures from one side of the brain to other. This is usually used with children who experience abnormal brain activity.
FIRST AID FOR EPILEPSY
It is important to know how to respond immediately when there is a person who is living with seizure. The first-line of response when a person has a seizure is to provide general care and comfort and keep the person safe.
WHAT TODOINTHE EVENT OF A SEIZURE
- STAY with person and start timing the seizure.
- Remain calm and check for medical ID.
- Turn the person onto their SIDE if they are not awake and aware. Don’t block airway, put something small and soft under the head, loosen tight clothes around neck.
- Do NOT restrain.
- Keep the person SAFE Move or guide away from harmful objects.
- Do NOT put anything in their mouth. Don’t give water, pills or food until the person is awake.
- STAY with them until they are awake and alert after the seizure.
Most seizures end in a few minutes. First aid for seizures is aimed at keeping the person safe until the seizure stops on its own.
FIRST AID IN FOCAL SEIZURE
In focal seizures, the person may appear unresponsive and confused as their consciousness is impaired. Automatic movements such as smacking of the lips wandering, or fumbling movements of the hand may be present. He or she may display inappropriate behaviour that may be mistaken for alcohol/drug intoxication or psychiatric disturbance. The instructions to be followed are:
- Keep the person away from obstacles and from dangerous places
- Keep calm and talk with the person as they regain awareness after seizure
- Reassure the person that they are safe and that you will stay with them while they recover.
FIRST AID FOR GENERALIZED TONIC-CLONIC SEIZURES
- Cushion head, remove glasses
- Loosen tight clothing
- Turn on side
- Time the seizure with a watch
- Don’t put anything in mouth
- Look for I.D.
- Don’t hold down
- As seizure ends …… offer help
FIRST AID FOR EPILEPSY PATIENT CONFINED IN AWHEELCHAIR, SEATED IN A BUS, TRAIN
DON’T
- Try to stop the seizure.
- Put anything in the person’s mouth.
- Try to remove them from their seat. In most cases the seat provides some support
DO’S
- Protect the person by preventing them from falling if there is no seat belt
- Make sure the wheelchair or the. Stroller is secure.
- Protect the person by supporting their head. Something soft under the head will help, if there is no moulded headrest.
- Check whether you need to move any hard objects that might hurt arms and legs in particular.
- Consciousness usually returns within a few minutes.
- Reassure the person and tell them what has happened.
First aid for seizures occurring in water
A seizure in water is a life-threatening situation. Loss of consciousness is especially dangerous and emergency care must go beyond the routine procedures. The steps to be followed, if someone is having a seizure in water e.g ., bath, swimming pool:
Support the person in the water with the head tilted so the face and head stay above the surface of the water. Remove the person from the water as soon as the active movements of the seizure have ceased.
Check if the person is breathing and whether they have a pulse. If they are Not breathing but have a pulse start mouth to mouth resuscitation and immediately call ambulance.
Even if the person appears to be fully recovered, call an ambulance.
Person should have a full medical check as inhaling water can cause lung or heart damage.
If a seizure happens out of the water during swimming activity, the person should not continue with swimming or water sports that day, even if the person appears to be fully recovered.
WHEN SEIZURE OCCURS IN A CROWDED PLANE MILES ABOVE THE EARTH, THE RULES FOR
FIRST AID ARE DIFFERENT.
- Clear space by folding up seat arms. Ask a flight attendant to find new seats for the other passengers in the row.
- Lie the person down across the seats with the head and body turned on one side.
- Make sure that the airway is clear, and breathing is not obstructed. Arrange pillows or blankets to prevent the person’s head from hitting unpadded areas.
- When the seizure stops, help the person into a resting position in a single reclining seat.
- If the seizure continues for more than about 5 minutes or is immediately followed by another one, tell the flight attendant that the person may be experiencing a medical emergency and may need emergency care.
EPILEPSY ANDCHILDREN
The diagnosis of epilepsy occurs most commonly in children under five. However, epilepsy can occur at any stage in childhood (or adulthood). Some epilepsy syndromes will appear in infancy and early childhood and can be recognized by other concomitant identifying factors from blood tests, cognitive ability and the appearance, type and number of seizures.
Seizures in children have many causes. Common causes of childhood seizures or epilepsy include:
- Fever (called as febrile seizures)
- Lack of oxygen to the brain
- Genetic causes
- Hydrocephalus (excess water in the brain cavities)
- Head injury
- Infections of the brain?
- Disorders of brain development
TIPS FOR PARENTS
- Discuss about epilepsy with all the family members and bring awareness
- Siblings may fear that the epilepsy is contagious. Reassure them that this is not true
- Encourage your child’s teacher to discuss epilepsy in the class, to make other students aware of your child’s seizures, if necessary Encourage the child to ask questions
- Explain which restrictions apply to the child with epilepsy
- Be honest with your child. The child should know that other people know she/he has epilepsy. Secret can make them feel ashamed
- Encourage your child to have as much a social contact with other children as possible and to participate in the activities.
- Meet with your child’s teachers to discuss your child’s epilepsy
EPILEPSY AT SCHOOL
Children with epilepsy going to school can be stressful. The child might be worried about having a seizure in class or how other students will react. Parents are also extremely worried that their child’s teacher may not know how to handle an epileptic seizure, or that their child may be treated unfairly because of epilepsy.
MANAGING EPILEPSY AT SCHOOL
- Educate the school nurse, teachers, staff, and students about epilepsy and what they should the do in the event of a seizure
- Follow the seizure action plan and administering first aid.
- Understand the importance of medication adherence and support students who take daily medications
- Help students avoid seizure triggers, such as flashing lights.
- Refer students with uncontrolled seizures to medical services.
- Monitor student behaviour to prevent bullying of students with epilepsy.
- Having a seizure at school can be embarrassing for a child and frightening for others. It is better if the teacher discusses it with students beforehand.
Sports and Other Extracurricular Activities
children with epilepsy can participate in most recreational activities and sports. these activities can enhance wellbeing and maintain health
activities to enjoy include
- tennis
- volleyball
- track and field jogging
- cross country skiing
- basketball
- hiking
- baseball
- golfing
- sports that pose some risk
- hockey
- soccer
- karate
- foot ball
- boxing
- activities that are considering dangerous
- scuba diving
- rock climbing
- parachuting
participation in recreational activities and sports should be discussed with the doctor
Children with epilepsy can participate, in most sports and social physical activities. Participation helps and promote positive self-esteem Encourages interaction and self-expression and supports physical and mental well-being. However, some special precautions should be taken into consideration.
GROUP ACTIVITIES
Group activities are part of childhood and encourage a sense of “belonging,” high self-esteem, and independence. These activities are usually well supervised. These benefits are extremely valuable, and usually outweigh the risk of injury.
SWIMMING AND WATER SPORTS
Swimming with a companion, preferably An experienced swimmer, is recommended for anyone who has seizures. If a person has uncontrolled seizures, then swimming is not advisable without constant supervision.
Before a child with epilepsy tries a new sport, discuss it with the epilepsy care team.
The school staff should be informed about the child’s condition and ensure they know what to do in case of a seizure.
Many sports require a helmet. This is especially important when child has epilepsy because a head injury can trigger seizure. The child should follow all the safety regulations of the sport.
EPILEPSY AND DRIVING
Driving a car is so critical to employment, socialization, and self-esteem that people with epilepsy list it as one of the main concerns.
seizures with motor and visual impairment, and with loss of consciousness, may pose greater risk than others. One immediate effect of having a seizure is that you have to stop driving. This is true for all types of seizures, and whether you have a diagnosis of epilepsy or not. For many people, this can have a big
impact on their life, and it may be very difficult or upsetting. People with epilepsy have an accident rate of between 1.13 and 2.16 times that of normal people
Epilepsy and travelling
Travelling is associated with lack of sleep, stress, anxiety, changes in diet and unfamiliar or increased sensory stimulation (lights or noise). These factors may trigger epilepsy attack. Further, during travelling the patient may forget to take medications.
- Get plenty of sleep before the trip
- Plan rest periods during each day
- Use sunglasses, sleeping mask and ear plugs whenever needed
- Keep medications in its original containers
- Carry enough medication to last the whole trip plus several days
- Letter that tells other people, what To do if there is seizure attack
- Always carry medications in handbag
- keep up normal daily meal times and sleep schedules
- avoid drinking coffee
- Wear a medical alert bracelet or ID
WORK ANDEMPLOYMENT
Having epilepsy does not necessarily stop someone from doing the job they want, but there some issues which them at work.
GUIDE TO EPILEPSY IN WORKPLACE
- Understand the nature of the person’s condition.
- Identify any triggers for their seizures, and work out how these can be eliminated or reduced to minimize the risk as much as possible.
- Understand the individual’s requirements during and after a seizure and ensure that appropriate provision is made,
- Consider allocating the person a dedicated locker to keep items needed during/after they have a seizure.
- Organize the individual’s work hours, tasks and pace to ensure: Targets and workload are manageable
- Driving is not required
- Shifts that might influence seizures or medication times are avoided
- At least one person who know first aid is present with the individual at all times
- Ensure the person has easy access to an accessible toilet and suggest they use it at all times.
EPILEPSY AND PREGNANCY
Epilepsy raises special concern especially during pregnancy. Most of the women with epilepsy can become pregnant, however there might be certain level of risks associated as compared to women without epilepsy. These risks can affect their health and that of their babies. If the epilepsy is managed properly then risks are small.
EPILEPSY DURING PREGNANCY CAN POSE A SERIOUS CHALLENGE. EPILEPSY CAN AFFECT PREGNANCY IN A VARIETY OF WAYS. EPILEPSY DURING PREGNANCY CAN CAUSE:
- Slowing of the fetal heart rate
- Preterm labor, premature birth
- Decreased oxygen to the fetus
- Miscarriage due to trauma experienced during seizures
- Fetal injury, miscarriage due to trauma, such as a fall, during a seizure
- Premature birth
- Most pregnant women who have epilepsy deliver their babies without complications.
- Epilepsy during pregnancy raises special concerns.
While most women who have epilepsy deliver healthy babies, you might need special care during your pregnancy .A daily prenatal multivitamin containing 0.4 mg folate, as well as an additional 2 mg folate supplement is recommended for all women of childbearing age.
Consider following tips to ensure the healthiest pregnancy possible.
- Preconception counselling should be done before planning a pregnancy
- Pay attention to healthy living and seizure triggers
- Get enough rest and sleep
- Pay attention to nutrition,
- With adequate weight gain
- Involve your spouse and family members support as early as possible!
EPILEPSY AND BREASTFEEDING
Breastfeeding is encouraged for most women who have epilepsy, even those who take anti-seizure medication. Breastfeeding to the new born offers advantages, like improvement in the baby’s health and immunity. Breastfeeding is an integral and important part of the experience of motherhood.
During breastfeeding the baby will get exposed to the seizure medication in varying concentrations depending on the prescribed AED. Usually this is only a small amount. However, the amount of medication present in breastmilk is less than the amount the baby was exposed to during pregnancy.
TIPS TO LESSEN THE AMOUNT OF MEDICATION THAT REACHES THE BABY:
Take AEDs once-a-day, that too at the beginning of the baby’s longest sleep interval, usually right after the bedtime feeding.
If you need to take your seizure medicine more than once-a-day, breastfeed the baby immediately before you take a dose. That’s when the level is likely to be lowest.
Supplement breastfeeding with formula at some feedings.

DR. RAVIRAJ S GHORPADE M.Ch(Neuro,NIMHANS)
CONSULTANT BRAIN & SPINE SURGEON
ADVANCED BRAIN AND SPINE SURGERY
BHS LAKE VIEW GROUP OF HOSPITALS -BELGAUM-10